Providing insights to counter medical deserts in Europe
Everybody wants to receive the healthcare they need, whenever and wherever they need it. However, medical deserts are increasingly hindering this. Medical deserts are areas where access to healthcare services is limited, for example due to a lack of health workers or a misalignment between the population’s health needs and the available services. This leads to long travel distances to healthcare services and/or hinders people in accessing quality and relevant healthcare in a timely manner. To tackle health inequalities in the European Union (EU), the European Commission has prioritized addressing medical deserts in their funding streams, stimulating EU member states to take appropriate action.
However, for EU member states to successfully address medical deserts, they first need to understand what medical deserts entail, and recognize that medical deserts are an urgent public health issue. Subsequently, they need more knowledge about potential policy solutions to effectively address these areas.
European project to learn about medical deserts and how to counter them
The Wemos-led Action for Health and Equity: Addressing medical Deserts project (AHEAD) addressed these needs. We gained insights into medical deserts and developed policy options to counter them. The European Commission funded our project and we worked with partners in Italy, Moldova, the Netherlands, Romania, and Serbia. Their expertise ranged from academic research to public health management to civic participation in policymaking.
Medical deserts
No medical desert is alike. They can be rural, geographically isolated areas that are difficult to reach for an ambulance or areas where people have to travel a long distance to visit a general practitioner. Yet, urban areas where health services do not align with the local population’s health needs, can also become medical deserts. What medical deserts have in common is that access to healthcare is not a given. In such areas, people’s health needs are continuously not met. This can exacerbate health inequalities, affecting vulnerable groups such as the elderly.
Medical deserts are a growing problem in Europe, hampering many European citizens to receive the healthcare they need.
Visualizing medical deserts to illustrate the problem
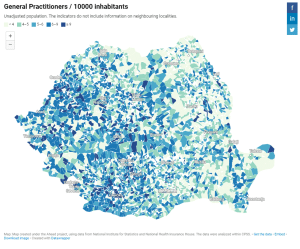
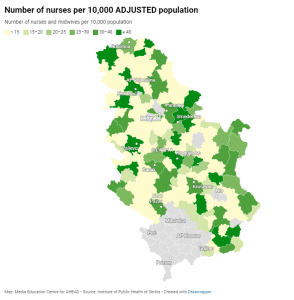
Through literature review, interviews and media analysis, we learned that medical deserts manifest in different ways in Italy, Moldova, the Netherlands, Romania or Serbia. The root causes for medical deserts differ. In general, these lie in demographic changes, such as an ageing general population and an ageing health worker population, corresponding increased and changing healthcare needs, as well as geographic concentration of specialty healthcare.
Because understanding and ‘seeing’ the problem was such an essential step to creating awareness for the problem, we developed a tool that visualizes medical deserts in each of the countries. This tool helped us show policymakers the extent of the problem and raise their awareness about medical deserts.
Waiting for an ambulance for more than two hours
During our project, we met Aleksander, a retiree in a medium-sized town in Serbia. He shared a story about his experience with the healthcare system. One day, after suspected nerve damage, he had to call his son for assistance because there was no ambulance available. His son contacted the emergency room at the public hospital, but was told to bring his father himself, “when he felt better”. Instead of accepting the situation, he arranged a visit to a private doctor and nurse, who provided care for his father. Being surrounded by buildings and living in a town with a primary healthcare facility, pharmacies, a public sector hospital and private health practices, Aleksander had never felt he was in a medical desert. But still, despite paying healthcare insurance, without the help of his son, his urgent medical problems would not be solved in Serbia’s public health sector.
We also met Maria, a 70-year-old resident of a rural town in the Campania region in Italy. She told us that when her friend fell and fractured her hip, she had to wait for over two hours with her for the ambulance because it was engaged in another emergency. Maria emphasized how important essential services like healthcare are in remote areas. “Even in optimal conditions”, she said, “without other emergencies and with good weather conditions, an ambulance takes about an hour to reach my village. If we do not want our beautiful ‘inner areas’ to become deserts, we must ensure that they offer opportunities for young people, and that essential services are available for everyone.”
Developing viable solutions with people in the field
To develop viable policy solutions to counter medical deserts, we held consensus-building workshops with local and national stakeholders in the five countries. The groups were diverse, with representatives from civil society and health associations, health advocates, and government level representatives, among others. We facilitated discussions about different solutions, aiming to reach consensus on a set of policy options at national and EU level.
In the workshops, we learned that solutions can only be effective if they are tailored to the local contexts and involve local, national and EU level stakeholders. A variety of (health workforce) policy solutions were proposed. These included recruiting more health workers for rural areas and improving their working and living conditions, implementing mobile pharmacies and clinics, and increasing cooperation between general practitioners and other healthcare providers, like geriatric specialists.
Both a national and a European issue to solve
A recurring symptom of medical deserts is the lack of health worker availability, in the right number, with the right skills. Health workers are key to offering good quality healthcare. Unfortunately, the availability of healthcare professionals differs widely across the EU. Insufficient training and ineffective or absent retention strategies are part of the cause. The EU’s free movement of workers also plays a role, although unintended; it enables healthcare workers to move to places with better career opportunities.
Stronger health workforce policies are needed to improve training, working conditions, recruitment and retention of health workers – not only at country level but also at EU level. Stronger EU action is essential, because the uneven health worker availability challenges the EU’s ambitions for shared prosperity and solidarity across its member states.
Therefore, we not only contributed to policy recommendations for member states, but ultimately also pushed for collective action by the EU itself. Considering the interconnectedness between members states and the EU, the EU should bear collective responsibility for the commonly felt health workforce crisis and develop an ambitious, overarching plan to counter it.
Elevating medical deserts on the EU agenda
To elevate medical deserts on the agenda at EU level, we organized a policy dialogue in the European Parliament in April 2023, bringing together people who experience medical desertification first-hand and policymakers. Acknowledging the need for joint action to tackle medical deserts, we urged the different actors to work together. We expressed several calls for action:
- For European institutions to:
a) encourage European Member States to use available data and tools to identify medical deserts, and
b) improve information and dissemination about funding mechanisms for investments in health, education and economy in areas with vulnerable populations and remote communities. - For member states to create a sustainable national strategy that addresses medical deserts and desertification.
- For education institutes to play a valuable role by continuously adapting health professionals’ education to population needs and health service requirements, with specific attention to remote areas.
- For health professionals associations to participate in the co-creation of policy solutions to ensure that they are contextually relevant and include effective incentives to work in areas that could be deemed as medical deserts.
- For citizens associations to participate in multi-stakeholder, co-creation processes for the development of policy solutions to healthcare challenges.
A common concern that requires joint action
All EU member states experience the challenges that come with health inequalities, medical deserts, and the health workforce crisis. They are all a common concern. We need to build robust and resilient health systems to overcome these challenges. But since health systems do not function in isolation from our internal EU market mechanisms, the EU should treat these challenges as a shared responsibility. The EU has policy instruments as well as funding at its disposal to tackle the challenges effectively. What it needs now is multi-sectoral collaboration and sustained efforts for many years to come.
Crucial steps to tackle medical deserts
We garnered a lot of attention for medical deserts with our AHEAD project. Policymakers increasingly acknowledge the need for a strong health workforce and the urgency to address problems related to health worker shortages and insufficient access to healthcare. We will continue building on our project results in policy discussions on the health workforce by engaging with EU stakeholders and closely following developments and conversations around medical deserts in Europe. Most importantly, we will emphasize the need for continued monitoring and evaluation of how member states use our insights and recommendations to ultimately achieve effective policy change.
The urgent health crisis in Europe cannot wait; tackling medical deserts is crucial to ensure that everybody receives good quality healthcare from skilled, motivated and properly supported health workers. Whenever and wherever they need it.